Owning a small business often means facing budget constraints and a heavy workload. However, neglecting to offer health insurance can negatively impact employee retention and overall workplace happiness. In the past, providing health insurance as a small business was challenging due to high costs and administrative burdens associated with traditional group health plans. However, with the introduction of Individual Coverage Health Reimbursement Arrangements (ICHRA), small businesses now have a more affordable and flexible option to provide health insurance to their employees. ICHRA allows employers to offer pre-tax funds that employees can use to purchase the health insurance plan of their choice, ensuring comprehensive coverage and increased employee satisfaction.
Key Takeaways:
- Small businesses face challenges in providing health insurance due to high costs and administrative burdens of traditional group health plans.
- Individual Coverage Health Reimbursement Arrangements (ICHRA) offer an affordable and flexible option for small businesses to provide health insurance.
- ICHRA allows employers to offer pre-tax funds that employees can use to purchase their preferred health insurance plan.
- Providing health insurance through ICHRA ensures comprehensive coverage and increases employee satisfaction.
- Choosing the right health insurance option is crucial for small businesses to promote a healthier workforce and happier employees.
The Challenges of Small Business Health Insurance
Small businesses face several challenges when it comes to providing health insurance for their employees. Traditional group health insurance plans, while popular among larger companies, present unique obstacles for small businesses to navigate.
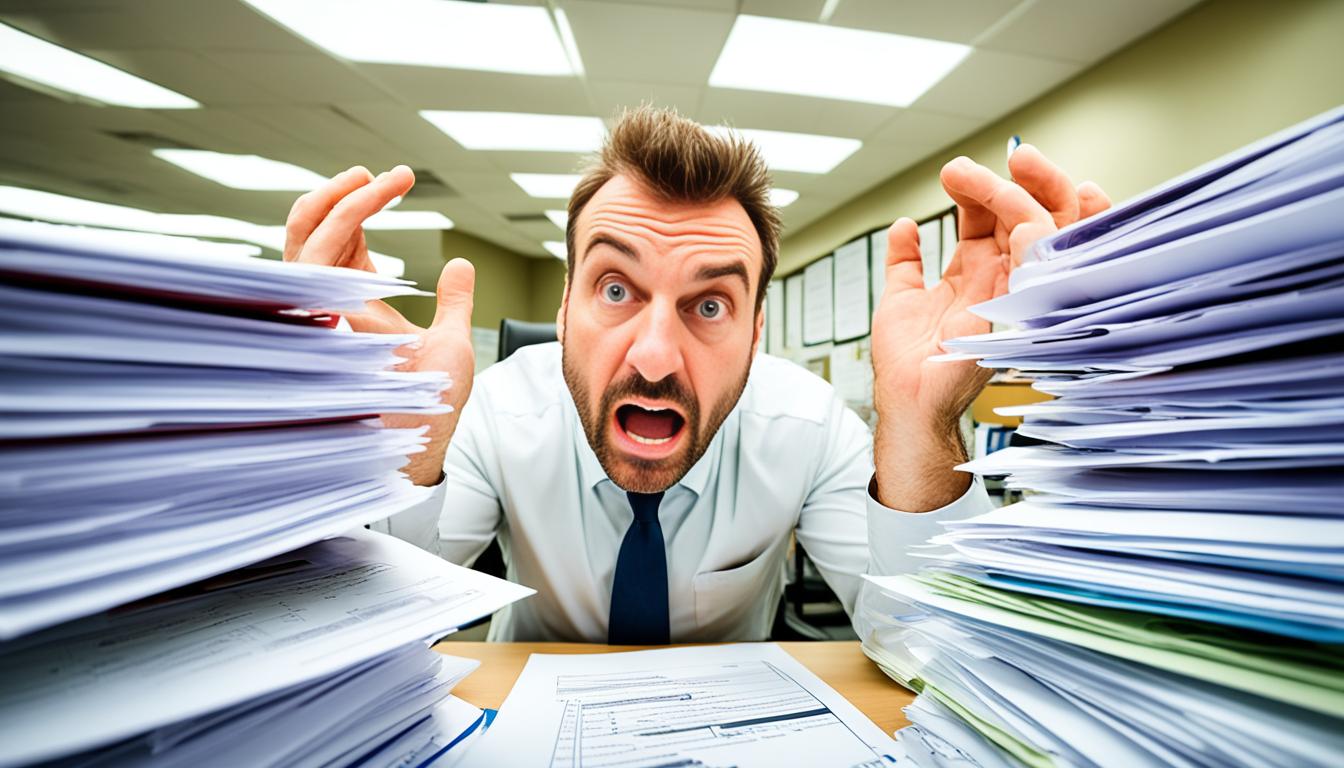
One of the main challenges is the significant time commitment required to set up a group plan. This process can often take more than 30 hours spread out over several weeks, demanding valuable time and resources from small business owners and their teams.
Additionally, most group plans have a minimum participation requirement, typically around 70%. This means that a certain percentage of employees must enroll in the plan in order for the business to qualify. Small businesses may find it difficult to meet this threshold, especially if they have a limited number of employees.
Another major challenge is the high costs associated with group health insurance premiums. On average, individual premiums can reach $8,435 per year, while family premiums can soar to $23,968 per year. These costs have been steadily increasing over the years, making it increasingly difficult for small businesses with tight budgets to afford comprehensive health coverage for their employees.
Overall, the challenges of small business health insurance include:
- Significant time commitment
- Minimum participation requirement
- High costs
Small Business Health Insurance Options
When it comes to offering health insurance, small businesses have three main options to consider. Let’s explore each option and discuss the advantages and challenges they present.
Traditional Group Health Insurance Plans
Traditional group health insurance plans are commonly associated with larger companies. While these plans offer comprehensive coverage, they can be challenging for small businesses due to their high costs and limited flexibility.
Small businesses often struggle with the financial burden of group health insurance premiums, which can strain their budgets. Additionally, these plans may not provide the flexibility required to meet the diverse needs of employees.
Cash Benefits
Another option for small businesses is to provide cash benefits to employees for purchasing their own health insurance. This approach allows for more flexibility, as employees can choose a plan that suits their individual needs.
However, it’s important to note that cash benefits may not always be seen as a true benefit by employees. Some may prefer the security and convenience of a traditional group health insurance plan.
ICHRA: Individual Coverage Health Reimbursement Arrangement
The introduction of ICHRA has revolutionized health insurance options for small businesses. ICHRA is a pre-tax health benefit that allows employers to allocate funds to employees, who can then use those funds to purchase their own health insurance plans.
This option offers affordability, flexibility, and ease of administration. Employees have the freedom to choose from a wide range of health insurance plans, ensuring coverage that suits their specific needs. For small businesses, ICHRA provides a cost-effective solution to offering health insurance benefits while minimizing administrative burdens.
Table: Comparing Small Business Health Insurance Options
| Options | Advantages | Challenges |
|---|---|---|
| Traditional Group Health Insurance Plans | – Comprehensive coverage – Security for employees |
– High costs – Limited flexibility |
| Cash Benefits | – Flexibility for employees – Reduced administrative burden for employers |
– Not universally perceived as a true benefit – Potential tax implications |
| ICHRA | – Affordability – Flexibility for employees – Ease of administration |
– Requires employee education on individual plans – Potential variation in coverage |
By exploring the available options and understanding the specific needs of their business and employees, small business owners can make informed decisions about providing the best health insurance coverage. The introduction of ICHRA has made it easier for small businesses to offer affordable and flexible benefits, ensuring the well-being of their employees.
Benefits of Group Health Insurance
Group health insurance plans offer numerous benefits for small businesses, despite the challenges associated with their implementation. These plans not only enhance employee recruitment and retention efforts but also ensure compliance with state and federal regulations. Additionally, group health insurance provides consistent costs, offering stability for both employers and employees.
Attracting and Retaining Employees
When it comes to attracting top talent, health insurance benefits play a crucial role in the decision-making process for job seekers. Group health insurance plans provide a valuable incentive for prospective employees, demonstrating that the company is committed to their well-being. Moreover, offering comprehensive health coverage through group plans also fosters employee loyalty and enhances retention rates, reducing turnover and associated recruitment costs.
Compliance with State and Federal Regulations
Group health insurance plans ensure compliance with state and federal regulations, particularly those outlined in the Affordable Care Act (ACA). These plans guarantee essential health coverage as defined by the ACA, including preventive services, maternity care, mental health treatment, and more. By providing group health insurance, small businesses not only meet legal requirements but also contribute to the overall health and well-being of their workforce.
Consistent Costs for Stability
One significant advantage of group health insurance plans is the consistent costs they offer. Once a plan is chosen, employers and employees can rely on predictable premiums and contributions throughout the year. This stability allows businesses to budget effectively, ensuring that health insurance expenses remain manageable and predictable. Moreover, employees can plan their finances with confidence, knowing that their health insurance costs will remain steady.
“Group health insurance offers small businesses the opportunity to provide attractive benefits, comply with regulations, and maintain stable costs for both employers and employees.”
Overall, group health insurance plans provide a range of benefits for small businesses. They are instrumental in employee recruitment and retention efforts, ensure compliance with state and federal regulations, and offer stability in terms of costs. By offering group health insurance, small businesses can prioritize the well-being of their employees while also enhancing their overall competitiveness and financial stability.
Issues with Group Health Insurance
The benefits of group health insurance plans for small businesses are well-known, but there are also several issues that need to be considered. Here are some of the main challenges that small businesses may face when it comes to group health insurance.
The high costs associated with group health insurance premiums can be a significant burden for small businesses. These costs can often exceed the budget of the business, making it difficult to afford comprehensive health coverage for employees.
Group health insurance plans also offer limited flexibility, as all employees are required to be on the same health insurance plan. This may not meet the individual needs and preferences of each employee, resulting in dissatisfaction and potential gaps in coverage.
Meeting the minimum participation requirements of group health insurance plans can also be challenging for small businesses. Employees may feel pressured to accept a plan that may not fully meet their specific needs, simply to meet the participation threshold.
Setting up a group health insurance plan requires a significant time commitment, which can be overwhelming for small business owners who are already juggling multiple responsibilities.
It is important for small businesses to carefully consider these issues when evaluating their options for providing health insurance coverage to their employees. Fortunately, there are alternative options available that address many of these challenges, such as Individual Coverage Health Reimbursement Arrangements (ICHRA).
Exploring Cash Benefits
Cash benefits offer small businesses a flexible approach to providing health insurance for their employees. Instead of enrolling employees in traditional group health plans, cash benefits give employees the freedom to choose their own health insurance plan using the money that would have been used for premiums. This allows employees to select a plan that best suits their individual needs and preferences.
By adopting cash benefits, employers can reduce administrative burdens associated with managing traditional group health plans. There is no need to enroll employees, choose a single plan, or manage ongoing plan changes. Instead, employers simply provide employees with the cash benefit and let them take the reins when it comes to selecting and managing their own health insurance.
However, it’s important to note that there are certain drawbacks to cash benefits. One key challenge is the perceived value of cash benefits as a true employee benefit. Since cash benefits are not directly tied to a health insurance plan, some employees may not view them as valuable or comparable to traditional group health insurance. Employers should communicate the benefits and flexibility of cash benefits to ensure employees understand their value.
“Cash benefits offer employees the freedom to choose their own health insurance plan.”
Another consideration is the tax implications of cash benefits for both employers and employees. When employers provide cash benefits in lieu of health insurance premiums, the cash is considered taxable income for employees. As a result, employees may be subject to FICA taxes and federal income taxes on the cash benefit, reducing its overall value. Employers should educate employees about the tax implications and work with tax professionals to ensure compliance.
In summary, cash benefits provide small businesses with flexibility in offering health insurance to their employees. This alternative approach allows employees to choose their own health insurance plan while alleviating administrative burdens for employers. However, employers should be aware of the potential challenges surrounding the perceived value of cash benefits and the tax implications for both parties involved.
| Pros | Cons |
|---|---|
| Flexibility for employees to choose their own health insurance plan | Perceived lack of value as a true employee benefit |
| Reduced administrative burdens for employers | Tax implications for both employers and employees |
The Introduction of ICHRA
ICHRA (Individual Coverage Health Reimbursement Arrangements) is a revolutionary option that small businesses can now utilize to provide health insurance benefits to their employees. This pre-tax health benefit allows employers to allocate funds that employees can use to purchase their own health insurance, offering affordability and flexibility.
Unlike traditional group health plans, ICHRA does not have any minimum participation requirements, giving employees the freedom to choose whether or not to participate. This flexibility ensures that employees have more control over their health insurance decisions, which can lead to increased satisfaction and engagement in their healthcare choices.
With ICHRA, employers also have the flexibility to offer different benefit levels based on employee status, whether they are part-time or full-time. This allows employers to tailor their health insurance offerings to the specific needs of their workforce, ensuring that employees receive the coverage that best suits them.
The Benefits of ICHRA:
- Pre-tax Health Benefit: ICHRA provides the advantage of offering pre-tax funds for employees to purchase health insurance, reducing their taxable income and potentially resulting in significant savings.
- Affordability: ICHRA offers small businesses an affordable option for providing health insurance benefits. Employers can set a budget based on what they can afford, avoiding the fluctuations in premiums associated with traditional group plans.
- Flexibility: With ICHRA, employees have the freedom to choose their own health insurance plan. This empowers them to select a plan that aligns with their individual needs, ensuring comprehensive coverage and increased satisfaction.
- Easy Administration: Unlike traditional group health plans with complex administrative requirements, ICHRA is relatively easy to administer. This allows small business owners to save time and focus on other important aspects of running their business.
By offering ICHRA, small businesses can provide their employees with a pre-tax health benefit that offers both affordability and flexibility. This innovative option allows employees to choose their own health insurance plan, giving them control over their healthcare decisions while ensuring comprehensive coverage. The introduction of ICHRA has truly transformed the landscape of small business health insurance, opening up new possibilities for both employers and employees.
Benefits of ICHRA
ICHRA offers several advantages for small businesses, providing predictable costs, clear health benefits, employee participation, plan flexibility, and time savings. Let’s explore each of these benefits in detail:
- Predictable Costs: Unlike traditional group health plans with fluctuating premiums, ICHRA allows employers to set a budget based on what they can afford. This ensures that businesses have predictable expenses related to health insurance.
- Clear Health Benefit: The money allocated through ICHRA is clearly designated for health insurance. This eliminates any confusion for employees and ensures that the funds are used specifically for their healthcare needs.
- Employee Participation: With ICHRA, participation is optional for employees. They have the freedom to opt-in or opt-out based on their preferences and personal circumstances, providing them with the flexibility and control over their health insurance choices.
- Plan Flexibility: ICHRA offers plan flexibility, allowing employees to choose the health insurance plan that best suits their specific needs. This ensures that employees can select a plan that covers the medical services and providers they prefer, providing them with personalized coverage.
- Time Savings: Offering ICHRA is less time-consuming compared to setting up a traditional group health plan. This frees up valuable time for small business owners, allowing them to focus on other core business activities.
Overall, ICHRA empowers small businesses to provide affordable and flexible health insurance options to their employees, ensuring predictable costs, clear benefits, employee participation, plan flexibility, and time savings.
| Benefits of ICHRA |
|---|
| Predictable Costs |
| Clear Health Benefit |
| Employee Participation |
| Plan Flexibility |
| Time Savings |

How to Find a Health Plan: The Marketplace
Employees who choose to take advantage of ICHRA will need to find an individual health insurance plan that is ACA compliant. The best way for employees to find such plans is through the health insurance marketplace. Any plan available on the marketplace is ICHRA-compatible and covers all essential benefits defined by the ACA, such as reproductive healthcare and prescription drug coverage. In Florida, some common health insurance carriers on the marketplace include Aetna, Ambetter, Florida Blue, Molina Healthcare, Oscar, and United Healthcare.
| Health Insurance Carrier | ACA-Compliant Plans Offered |
|---|---|
| Aetna | Gold, Silver, Bronze Plans |
| Ambetter | Gold, Silver, Bronze Plans |
| Florida Blue | Gold, Silver, Bronze Plans |
| Molina Healthcare | Gold, Silver, Bronze Plans |
| Oscar | Gold, Silver, Bronze Plans |
| United Healthcare | Gold, Silver, Bronze Plans |
Health Insurance Costs in Florida
When considering health insurance plans in Florida, it’s important to understand the different cost options and coverage levels available. These plans are categorized into gold, silver, and bronze levels, each offering varying degrees of coverage and corresponding premiums.
Gold plans provide the highest level of coverage but come with higher premiums. These plans are ideal for individuals who require comprehensive medical services and are willing to pay a higher monthly premium in exchange for lower out-of-pocket costs.
Silver plans offer a balanced approach, providing moderate coverage at more affordable premiums. These plans are suitable for individuals who want a reasonable level of coverage and are comfortable with a slightly higher out-of-pocket cost.
Bronze plans are the most cost-effective option, featuring lower premiums but less coverage. These plans are suitable for individuals who are generally healthy and have minimal healthcare needs, as they offer basic coverage with higher out-of-pocket costs.
When shopping for health insurance on the marketplace, employees in Florida can choose from a wide variety of plans within these categories. This allows them to find a plan that not only fits within their budget but also meets their specific coverage needs.
| Plan Level | Coverage | Premiums |
|---|---|---|
| Gold | Comprehensive coverage | Higher |
| Silver | Moderate coverage | More affordable |
| Bronze | Basic coverage | Lower |
Best Practices for Group Health Insurance Renewals
When it comes to group health insurance renewals, it’s essential to follow best practices to ensure a smooth and successful process. By implementing the right strategies, small businesses can effectively manage their group health insurance renewals, ensuring optimal coverage for their employees.
Start Early
The key to a successful group health insurance renewal is to start the process early. It is recommended to begin at least 90 days before the policy’s renewal date. Starting early allows ample time to review the current plan, assess employee needs, and explore alternative options.
Review Current Plan
Before renewing the group health insurance plan, it’s crucial to thoroughly review the current plan. Assess its effectiveness, cost, level of coverage, and employee satisfaction. Look for areas where improvements can be made to meet the changing needs of the workforce.
Assess Employee Needs
Taking the time to assess employee needs is crucial for a successful renewal. Understand what benefits are important to employees and if the current plan aligns with their expectations. This assessment will help tailor the plan to better suit the needs of the workforce.
Explore Options
During the renewal process, it’s essential to explore different options available in the market. Research other group health insurance plans, consider alternative insurance providers, and evaluate new coverage options that may better meet the requirements of the business and its employees.
Communicate with Employees
Clear communication with employees is vital throughout the renewal process. Keep employees informed about any changes to their health insurance plan and how it might impact them. Ensure they have the necessary information to make informed decisions and understand the benefits being offered.
Seek Professional Help
Renewing group health insurance can be complex, especially for small businesses with limited resources. Seeking professional help, such as an insurance broker or consultant, can provide valuable guidance and support. These professionals can navigate through the intricacies of group health insurance, ensuring the best possible coverage for employees.
Implementing these best practices will help small businesses streamline their group health insurance renewals. By starting early, reviewing the current plan, assessing employee needs, exploring options, communicating with employees, and seeking professional help, businesses can ensure they find the right coverage for their employees, fostering a healthier and more satisfied workforce.
Beware of Harmful Broker Practices
While most brokers have their clients’ best interests at heart, it’s important to be aware of harmful broker practices that may negatively impact a company’s health insurance quality and costs.
Some brokers may present limited options, favoring certain insurance companies with whom they have relationships or from whom they receive higher commissions. This can restrict the choices available to small businesses and prevent them from finding the best coverage for their employees.
Lack of transparency regarding fees and commissions can also be a problem. When brokers are not open and upfront about the financial arrangements they have with insurers, it can lead to unexpected costs and dissatisfaction among employees.
Inadequate support from brokers can leave employers struggling to navigate complex insurance issues on their own. Brokers who are unresponsive to questions and concerns can make it difficult for small businesses to understand their coverage and make informed decisions.
Brokers are vital partners in the health insurance process, but it’s crucial to work with professionals who prioritize transparency, provide a wide range of options, and offer responsive support.
Why Transparency Matters
Transparency is essential in broker-client relationships for several reasons:
- It allows small business owners to fully understand the costs associated with their health insurance plans and make informed decisions that align with their budgetary constraints.
- Transparency ensures that employees are aware of any potential conflicts of interest the broker may have, allowing them to fully trust that their best interests are being served.
- Clear communication around fees and commissions helps small businesses avoid unexpected costs and ensures that the broker’s compensation is fair and reasonable.
The Importance of Support
Adequate support from a broker is vital for small businesses navigating the complex world of health insurance.
- Responsive brokers can address questions and concerns promptly, providing clarity and peace of mind to employers and employees.
- Brokers who take the time to understand the unique needs of a small business can help identify the most suitable health insurance options and guide decision-making.
- Supportive brokers can assist with claims management, policy renewals, and other administrative tasks, saving time and effort for small business owners.
Protecting Your Business
To protect your business from harmful broker practices, consider the following:
- Research and choose brokers with strong reputations and a track record of transparency, customer satisfaction, and support.
- Ask for referrals from trusted business partners or industry associations.
- Have open and honest conversations with brokers about their fees, commissions, and relationships with insurance companies.
- Seek written agreements that outline the services provided and the compensation structure.
- If concerns arise, don’t hesitate to seek a second opinion or switch to a different broker who better aligns with your business’s needs.
| Issues | Consequences |
|---|---|
| Limited Options | Small businesses may not find the best coverage for their employees, leading to dissatisfaction and potential recruitment challenges. |
| Lack of Transparency | Unexpected costs can strain a small business’s budget, and employees may lose trust in the company’s health insurance offering. |
| Inadequate Support | Employers may struggle to navigate complex insurance issues, resulting in compliance risks and potential legal consequences. |
Conclusion
Navigating group health insurance options for small businesses requires careful consideration of the available choices and an understanding of the specific needs of the business and its employees. While traditional group health insurance plans have their advantages, they may not be the most feasible or cost-effective option for small businesses. Cash benefits can provide some flexibility but may not be seen as a true benefit by employees. ICHRA offers a viable alternative, providing affordability, flexibility, and ease of administration. By starting the renewal process early, reviewing the current plan, and seeking professional help if needed, small business owners can ensure that they find the best health insurance coverage for their employees, promoting a healthier workforce and happier employees.
FAQ
What are the challenges of small business health insurance?
Small businesses often face challenges such as high costs, limited flexibility, time commitments, and minimum participation requirements associated with traditional group health insurance plans.
What options are available for small business health insurance?
Small businesses have three main options: traditional group health insurance plans, cash benefits, and Individual Coverage Health Reimbursement Arrangements (ICHRA).
What are the benefits of group health insurance?
Group health insurance offers advantages such as attracting and retaining employees, compliance with state and federal regulations, and consistent costs throughout the year.
What are the issues with group health insurance?
Issues with group health insurance include high costs, limited flexibility, minimum participation requirements, and the time commitment required to set up a group plan.
What are cash benefits for small business health insurance?
Cash benefits involve providing employees with a set amount of money to purchase their own health insurance, offering flexibility but potentially lacking perceived value as a benefit and carrying tax implications.
What is ICHRA?
ICHRA is a pre-tax health benefit that allows employers to allocate funds for employees to purchase their own health insurance, offering affordability and flexibility.
What are the benefits of using ICHRA?
ICHRA provides predictable costs, clear health benefits, optional employee participation, plan flexibility, and time savings for small business owners.
How can employees find health insurance plans compatible with ICHRA?
Employees can find ACA-compliant health insurance plans compatible with ICHRA through the health insurance marketplace, which includes carriers such as Aetna, Ambetter, Florida Blue, Molina Healthcare, Oscar, and United Healthcare.
How are health insurance costs categorized in Florida?
Health insurance plans in Florida are categorized into gold, silver, and bronze levels, with gold plans offering the highest coverage and premiums and bronze plans offering the lowest coverage and premiums.
What are the best practices for group health insurance renewals?
Best practices for group health insurance renewals include starting the process early, reviewing the current plan, assessing employee needs, exploring alternative options, and communicating with employees throughout the process. Seeking professional help, such as an insurance broker or consultant, can also be beneficial.
What harmful practices should small businesses be aware of when working with brokers?
Small businesses should be cautious of brokers who present limited options, lack transparency regarding fees and commissions, and provide inadequate support and responsiveness.
What is the conclusion regarding small business health insurance?
Navigating group health insurance options for small businesses requires careful consideration of available choices, with options such as traditional group plans, cash benefits, and ICHRA offering different advantages and drawbacks. Small business owners should assess their specific needs and consider factors such as cost, flexibility, and administrative ease to find the best health insurance coverage for their employees.